Managing Back Pain: “your tool box to understand and fix things”.
Learn all about Back Pain, Chronic Back Pain and Perception of Pain from Tony Gill
What is lower back pain (LBP)?
This should be a simple answer with our medical technology to answer but pain is incredibly complex.
At times, physical changes and adaptions can increase our perception of pain but in itself is not enough to explain pain. MRI investigations point to many people with significant mechanical changes but with no pain. Then other people with minimal or no obvious changes have far higher pain. See more about MRI guidelines here.
We do know that stress , culture and socio-economics do correlate with reported back pain. Its is more helpful to think of back pain as a large complex jigsaw unique for every person. There are lots of elements that when added together can increase perception of pain.
Let’s start with physical. We know that as we age the back ages. The discs slowly dehydrate just like our skin does therefore no amount of rehydrating in the day alters this. As the discs dehydrate they flatten and bulge.
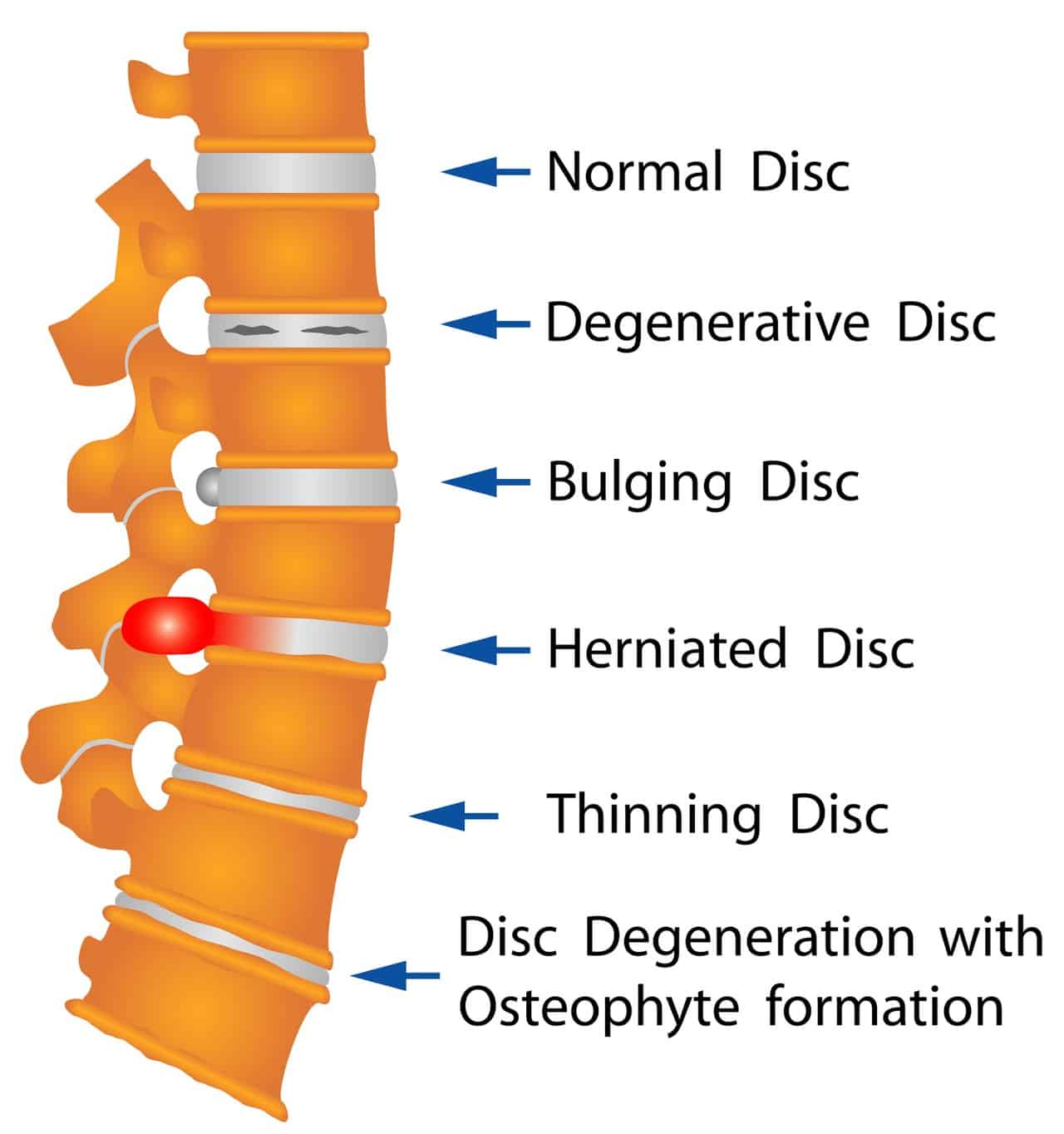
The joints then sit closer together and need to take more load. They are made of bone and have an amazing property to adapt. The joints thicken and bulk up to handle the bigger load. Normally all of this happens at a very slow rate, like your own body’s stalactites and stalagmite’s. The body tends to be happy with slow change and not as happy with rapid change. Slow change allows progressive adaption in the ligaments and muscles to cope with the change.
Rapid Change:
At times the change is too rapid or we injure and flare an area of change or the change our body is not able to cope with. This can lead to decreased movement and a perception of pain. It is important to stress that these changes happen to all of us over time and consequently are not unusual and do not have to cause pain.
I’ve been qualified for 18 years now and the longer I do this, my professional view is that pain tends to be linked to the body’s inability to adapt to rapid or sudden change. Rapid physical, mental, and emotional changes are all part of the jigsaw of LBP. Indeed these rapid stress changes can be on any aspect of our lives that cannot cope with rapid change.
Let’s look at acute LBP.
Injury and fitness:
This tends to be linked to a sudden movement or trauma. A car accident would be a good example where we were fine before but then have pain after. Interestingly there is a great study on neck pain in the police who suffered an RTA while at work. While it’s no surprise to see the acute trauma caused neck pain, those police who had higher pre fitness scores on their annual fitness test had less reported pain and consequently returned to work far more rapidly.

Thus pain, injury and physical fitness have a correlation. If we remain fit and well, we are potentially more likely to get over an injury quickly. We can even have an accelerated repair time i.e. have less of an injury or less pain perception. This means less pain perception.
Reducing pain:
We would expect acute back pain to settle within 6-8 weeks normally with or without medicine. Pain medication does not heal the injury, it can allow us to feel more comfortable. By reducing the pain we are more likely to move allowing the body to pump blood nutrients and oxygen to the area that needs to be repaired. The muscles also stay working, furthermore can add stability to the area that is injured. We are also able to heal with correct tension and loading thus the repair is optimal.
What happens with acute back pain when we get stuck or cannot move?
This tends to be due to muscle spasm that is guarding and protecting an area. Spasm stops movement while the system works out if the area is badly injured or if its ok to start moving. Previous experience of significant pain will heighten this guarding response. The system “is nervous” or has “pre-experience” of a bad experience and thus can be more wary.
In these circumstances, inappropriate guarding response and pain that is far in excess of the injury can occur. Getting the body moving, if this is the case, is very important if we are to break this cycle rapidly. Physio can help assess if this is a simple guarding. It can teach you what to do to get moving and positions to increase movement or decrease that flare.
My advice in acute pain:
- Take pain medication in the short term to allow for early movement.
- Listen to the body.
- Get moving as soon as possible within sensible limits.
Acute back pain with leg pain.
This is common and called sciatica.
If the leg pain is a lot worse than the back, but the bladder and bowels work normally and the groin and saddle area has normal sensation – with the leg not dramatically weak – 80% of these tend to settle in 6-12 weeks.

Physiotherapy can help teach you how to manage this in the short term. Your body will repair and adapt to settle the nerve flare in the vast majority of these cases.
Usually this leg pain is due to a chemical or mechanical compromise to one of the nerves in the back as it is getting ready to leave the spinal canal. Over time the body will heal thus adapt for this change.
Quite often things are irritated with sitting and static positions and easier moving.
Again listen to the body, don’t sit for too long and move! Gentle exercise again can promote healing and reduce guarding spasm pain that will flare things.
Pain medication can be adapted to include nerve modifying drugs. They do have potential noxious side effects so not everyone uses these. The medicine does not cure but humours the body while time settles things!
Chronic back pain:
This effect many of us upright monkeys and usually worse when we have been static for too long or spent too long bending over.
It is important to realise just because you feel pain it does not mean you are damaging yourself. Pain and damage are not the same thing.
Physio’s tend to be very good at ruling out the serious or worrying symptoms and reassuring you its ok to move and get active. If your worried book an appointment
If you have had pain for a long time the body adapts negatively. Muscles shorten and tighten, others lengthen and weaken. The ligaments are put under more stress and this changes the forces in the joints and discs.
This itself can lead to mal-adaptation that is negative for the system; i.e. the hips becoming tighter, consequently you walk with less speed. Stride length or frequency will then add further loading to the spine and can flare things
Quite often making the hips, pelvis and legs stronger and more able to take the load can have very beneficial effects on back pain.

Pelvic Power & Stability:
I tend to think of the hips and legs like a mountain bike shock absorber. You can have a cheap front shock that’s all show and no go! You can have an expensive front shock that works very well and takes lots of the impact out of trail as you bump down. Trust me as a regular MTB rider a good front shock makes a massive difference. Your comfort speed and enjoyment all improve. Your back will feel the same if you keep the legs hips and pelvis strong and able.

The trunk muscles are also important as these stabilise the spine while the rest of the body moves ie the arms and legs.
Chronic pain weakens these muscles and on MRI we can even see fat infiltration into them as they switch off in the long term. Building these back up requires time effort and hard work. There is no way around this if you are trying to optimise your back health.
Personally I think a lot of these “core” exercises can be done at the same time as general exercise. For example running can switch on these muscles beautifully and is how they learned to be strong in the 1st place. I understand it might be unrealistic to run or start running for many people with back pain and why good physiotherapy is important.

Brain effects: Our Perception of Pain
Right let’s get on with the fascinating bits now.
Brain scans of people with chronic back pain show grey matter changes. The brain had remodelled and adapted to the pain. This might mean the brain is actually perpetuating the pain more than the structures themselves.
This could mean you get fit and strong but still don’t get any relief in your perception of pain. Completely unfair right! Well that’s again where a good physio comes in as we can also train the brain to adapt the grey matter back to a more normal level.
Mindfulness:
Breathing exercises, mindfulness, meditation and other brain activities can help. Before you poo poo this, just remember how many top athletes and martial art masters spend hours in meditation. They are able to alter their perception of pain or discomfort.
This might be physical movement meditation. For example: repeating the same task again and again, holding a stance or practising a ski jump, a bike trick, a sprint. It might be resting meditation sitting or lying down.
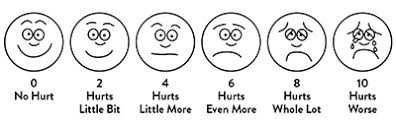
CBT and ACT therapies are just 2 models that help us change the synapses in the brain. This can help stop them firing in a negative pattern that flares the pain state. Simply lying down and deep breathing x 10 times from the diaphragm can reduce pain by up to 30% on a pain score. This allows the body and brain to settle together. This can significantly reduce perception of pain.
So what is the pain I’m feeling?
Have you ever poked a bruise? It’s more painful than poking the area of the body next to the bruise right? Therefore it’s in a sensitised state giving a perception of pain.
Pain is anything that can increase sensitivity:
* Physical inflammation, like the bruise
* Damage to the local nerve
* Changes to the central nerve from the spine up to the brain
* The brain itself
We do not have pain receptors or pain nerves. Just information going up and down that is interpreted by the central processing unit or brain. Incredibly frustrating at times but understanding this on a personal level will assist insight into the aspects of life that flare your experience of “pain”.
While I’ve already said it above, it’s really important to re-emphasise that very rarely does pain mean damage in LBP.
Translating the pain message:
If I hold a heavy weight out to the side in my arm after 30-60 seconds my arm will tire. If I continue to hold by the time my body gives up I will have the perception of pain.
It isn’t damage, its fatigue.
People who train their body to full fatigue on a regular basis will enjoy this feeling. They call it a fatigue or muscle burn and perceive it as a good sensation.
Similarly if I hold an aggressive stretch in my leg for too long the muscles and ligaments will at some point protest. I would be very unlucky to have caused any real damage, but I might perceive pain.
People who stretch on a regular basis might like this feeling. For them is a nice strong stretch sensation. This is like the old saying “one man’s meat is another man’s poison”. It is about perception of pain not damage.
Chronic weakness, muscle shortening and stabilising muscle fat infiltration combined, has a far higher chance of central brain changes. All of this together = reasons for chronic pain.
Sometimes we all need to take an internal step back and ask our body what information is the pain telling us. Usually it is saying ” I’m tight or fatigued” and gives us clues how to reduce the pain perception.
Fat effect!
Let’s be clear, being fat or having extra fat is not itself correlated with back pain.
To me, fat is load and load makes your muscles stronger.
A bigger person is usually stronger and legs are able to push more weight, but it’s all relative to strength relative to your size.
We do have a correlation with increased chronic back pain reported when people have raised central obesity. This also correlates to Diabetes, stroke, heart attack, arthritis and many other conditions.
We do know that central fat around the organs produces a hormone called Leptin. This acts as an appetite suppressant.
But when we have an excess the system becomes jaded “crying wolf” and the body becomes ‘leptin resistant’. We need to produce even more leptin to supress the appetite.
Why is this important, well Leptin is inflammatory. There are many models showing increased arthritis with high leptin levels. In one study up to 38% more severe knee OA with high serum levels of leptin in the joint.
My professional view is that fat increases inflammation. If you have a chronic back pain and changes, the last thing you need is more inflammation. This can make the system flare even more. It could be the difference between your back being a dormant volcano to an active erupting volcano!
This means sensible living, eating well with far less processed food. Eating less sugars and less simple carbohydrates that just turn rapidly to sugar. This should help you fuel with healthy foods for the long term.
Sleep:
I cannot over-emphasise how important sleep is to regulate your body and brain. Lack of sleep is correlated with shorter life span. It increases perception of pain and generally makes us all grumpy and annoyed.
Sleep hygiene is an important concept. Turn off that phone in the evening and less late night TV. Try good relaxation patterns i.e. read a book, listen to some music. Try communicating with the family if you live with one, play cards in the evening for example. Family meals without phones eating and talking together. Staying up late on screens is definitely detrimental to your health. We all know this on a deeper level.
What if pain is keeping you awake?
- Again physio can advise on tricks to help with positions in bed
- Pain medication to allow a better sleep are important.
Circadian Rhythm:
While I don’t get the luxury of a siesta, in hot climates this is different. The day time mid -day nap after food can be a great refresher.
For many in chronic pain, sleeping in the day and not sleeping at night is not beneficial. It can build a cycle of even worse pain patterns and is to be avoided.
So what helps us sleep better apart from less screen time and a sensible bed time?
Guess what? its exercise. Exercise is a super drug.
But more of that in a minute. Many studies show that having a good level of exercise in the day will help with sleep patterns.
If you sleep well:
- you will have more energy
- be in less pain
- be more able to face the day.
Exercise:
Yes I am biased to exercise as most physios are. We have countless studies showing exercise:
- Improves physical health
- Reduces risk of dementia,
- Reduces heart attack
- Improves Stroke risk
- Lower Obesity
- Is a powerful tool in depression management
- Improves sleep cycles.

Exercise is a pain killer, helping the body produce natural opioids reducing perception of pain. It’s a wonder drug and it’s free! If you’re not taking this drug you need to start right now.
It’s as essential to the human body as water, breath and food. If we want to have a long and happy life, with less pain and more independence. Why would you not take this medicine?
Exercise versus Active:
Now exercise does not have to be “gym kit, hamster wheels and weights” . If that’s your thing then great. Whatever you enjoy, we can advise a prescription of different exercises to target weakness and tightness. This will allow you to maximise your individual body and its mal-adaptation’s.
Exercise can also be an activity. Just measure a cleaners daily effort for example so cleaning a house can be exercise. Walking to the shop instead of driving and carrying the shopping back are your gym weights.
Let’s go back to our bodies design, we were a hunter and gatherer roaming and running across large stretches of land daily hunting in season and carrying the game back or foraging, fishing. It you don’t want to do formal exercise try being more active but if you walk, make it with purpose!
Posture:
For some people certain postures will increase or decrease their back pain.
Please listen to your body, if it says get up and move then get up and move. If it says I’ve been static for too long and I’m aching then move. If it says I’ve been moving too long it’s ok to sit and rest.
The message you are receiving is not of acute damage but the body asking you to change things.
Now here is the hard part. Sometimes the message is wrong i.e. the brain remembering what it was like last time you had an acute flare. It remembers it used to hurt to sit for too long. You have to take these messages with a pinch of salt.
Generally if you are progressively unable to sit or stand or walk for a period of time you need advice. If this is getting worse then you need help and advice to find a way to manage this.
If it’s an acute flare, listen to the body, change the position and take medicine to keep the muscles working. In chronic pain if you know your limit walk is 2 miles then listen to the body. If doing more flares you for days don’t do it “yet”.
Find a way of building the muscles, use walking poles , modify and use a bike or cross trainer etc. These are all reasons to get a physio involved.
My last bit on posture is to say sitting at a laptop or PC for hours on end is not your bodies design. Optimising this can help you reduce tightness weakness and core strength.
If I could get all of you using a sit stand desk and laptop docking stations I would!
“Exercise snacks”
Gemma one of the fab physio’s I work with who is also interested in chronic pain. She introduced me to this term and I love it.
We know for many people with chronic pain they have a boom-bust cycle. Basically they do too much and then crash into a cycle of increased pain. Does this sound familiar?
To avoid this perpetual cycle and perception of pain, it’s important to try doing small amounts little and often. Build a tolerance to load and exercise. You can then increase this over time rather than stuck in the perpetual boom/bust cycle.
While it’s easy to write about, living with pain that has a massive limitation in daily function. I fully appreciate it can have a huge impact on you and your family.
Stress Kills:
We know stress levels can cause heart attack, stroke, mental health conditions, sleep deprivation and back pain. The single highest reason for reported back pain when we do the stats is not physical damage… it’s Stress.
A certain amount of stress on the physical and mental state is healthy and lets us learn and adapt. To much is definitely a problem and large predictor for back pain.
Therefore finding a way of managing this is crucial to improving back pain in the long term for all of us.
Pieces of the Jigsaw:
* Sleep
* Exercise
* Bite size management
* Mindfulness
* Positive living
The above are all ways to help with this but don’t ignore stress as it effects all of us.
Final words
So I hope this Blog gives you more insight into lower back pain. Improving this and your quality of life for the long term is in your hands. Physio can help you on this journey. Our roll is to teach you and empower you in managing your back pain. The more tools you have and understanding how to use them will turn you into the expert. This means it is you in the drivers seat managing your back. Good luck !
